Thoát vị đĩa đệm tiếng anh là một tình trạng sức khỏe phổ biến, ảnh hưởng đến hàng triệu người trên toàn thế giới. Tình trạng này xảy ra khi phần mềm bên trong đĩa đệm cột sống thoát ra khỏi lớp vỏ bên ngoài, gây ra đau và các triệu chứng khác.
Trong bài viết này, chúng ta sẽ khám phá mọi thứ về thoát vị đĩa đệm tiếng anh, từ nguyên nhân và triệu chứng đến các lựa chọn điều trị và phòng ngừa.
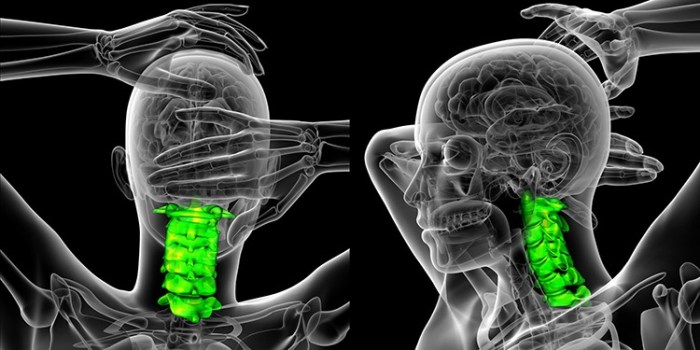
Thoát vị đĩa đệm có thể ảnh hưởng đến bất kỳ phần nào của cột sống, nhưng phổ biến nhất là ở vùng thắt lưng và cổ. Tình trạng này thường xảy ra do quá trình lão hóa tự nhiên, chấn thương hoặc các hoạt động lặp đi lặp lại gây căng thẳng cho cột sống.
Các triệu chứng của thoát vị đĩa đệm có thể bao gồm đau, tê, ngứa ran và yếu ở các khu vực của cơ thể được chi phối bởi các dây thần kinh bị ảnh hưởng.
Definition and Overview of Disc Herniation

A disc herniation, also known as a slipped disc or ruptured disc, occurs when the soft, jelly-like center of an intervertebral disc pushes through the tough outer layer. Intervertebral discs are located between the vertebrae, the bones that make up the spine.
They act as cushions, absorbing shock and allowing for movement of the spine.
Disc herniations can occur in any part of the spine, but they are most common in the lower back (lumbar spine) and neck (cervical spine). When a disc herniates, it can put pressure on the surrounding nerves and spinal cord, causing pain, numbness, and weakness.
Types of Disc Herniations
There are several different types of disc herniations, depending on the location and severity of the herniation. Some of the most common types include:
- Posterior herniation:This is the most common type of disc herniation, and it occurs when the disc material pushes backward into the spinal canal.
- Lateral herniation:This type of herniation occurs when the disc material pushes sideways, either to the left or right.
- Foraminal herniation:This type of herniation occurs when the disc material pushes into the foramen, the opening through which the spinal nerves exit the spinal canal.
- Central herniation:This type of herniation occurs when the disc material pushes directly backward into the spinal canal, compressing the spinal cord.
Prevalence and Risk Factors
Disc herniations are a common problem, affecting up to 10% of the population. They are most common in people between the ages of 20 and 50. Some of the risk factors for disc herniations include:
- Age:The risk of disc herniation increases with age as the discs become less flexible and more prone to tearing.
- Occupation:People who do heavy lifting or have jobs that require them to sit for long periods of time are at an increased risk of disc herniations.
- Obesity:Excess weight puts extra pressure on the discs, increasing the risk of herniation.
- Smoking:Smoking damages the discs and makes them more likely to herniate.
- Genetics:Some people are more likely to develop disc herniations due to their genes.
Causes and Symptoms of Disc Herniation: Thoát Vị đĩa đệm Tiếng Anh
Disc herniations are caused by a variety of factors, including aging, genetics, and lifestyle choices. As we age, the discs in our spine begin to lose their water content, which makes them more susceptible to tearing. In addition, certain genetic factors can also increase the risk of disc herniation.
Finally, lifestyle choices such as smoking, obesity, and heavy lifting can put additional stress on the discs in our spine, increasing the likelihood of a herniation.
The symptoms of a disc herniation can vary depending on the location of the herniation. However, some of the most common symptoms include pain, numbness, and weakness in the back, neck, or extremities. In some cases, a disc herniation can also cause problems with bowel or bladder function.
Mechanism of Pain, Thoát vị đĩa đệm tiếng anh
A herniated disc can cause pain by compressing the nerves that run through the spine. This compression can irritate the nerves, causing them to send pain signals to the brain. In addition, the herniated disc can also put pressure on the spinal cord, which can lead to further pain and neurological problems.
Diagnosis and Imaging for Disc Herniation

Diagnosing disc herniations involves a combination of physical examinations and imaging tests. Physical examinations can provide valuable information about the location and severity of the herniation, while imaging tests offer detailed anatomical images to confirm the diagnosis.
Physical Examination Techniques
- Neurological Examination:This assesses nerve function, including sensation, reflexes, and muscle strength, to determine which nerves are affected by the herniation.
- Straight Leg Raise Test:The patient lies on their back, and the examiner lifts one leg while keeping the knee straight. Pain or numbness in the leg may indicate a herniation affecting the sciatic nerve.
- Kernig’s Sign:The patient lies on their back with their hips flexed and knees bent. The examiner attempts to extend the knee, causing pain in the lower back if there is a herniation.
Imaging Tests
Imaging tests provide detailed anatomical images of the spine and can confirm the presence, location, and severity of a disc herniation.
- X-rays:X-rays provide images of the bones and can show narrowing of the spinal canal or misalignment of the vertebrae, which may indicate a herniation.
- Magnetic Resonance Imaging (MRI):MRI uses strong magnets and radio waves to create detailed images of the soft tissues, including the discs and nerves. MRI is the most accurate test for diagnosing disc herniations.
- Computed Tomography (CT) Scan:CT scans use X-rays and computers to create cross-sectional images of the spine. CT scans are less detailed than MRI but can provide useful information about bone structures.
Interpretation of Imaging Results
Imaging results are interpreted by a radiologist, who will provide a report to the physician. The report will describe the location, size, and severity of the herniation. The physician will then use this information to determine the best course of treatment.
Conservative Treatment Options for Disc Herniation
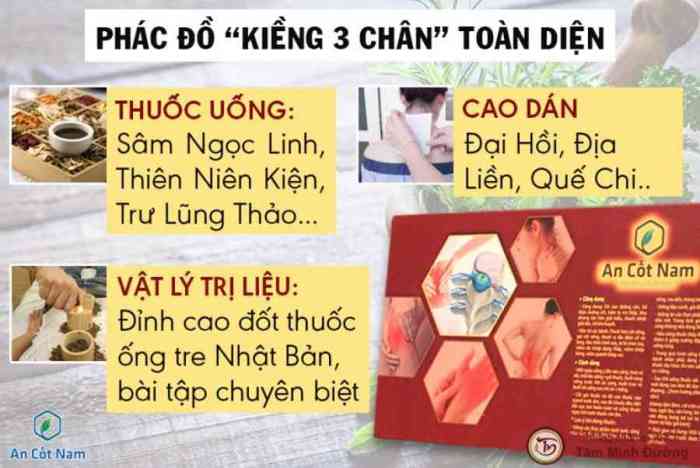
Conservative treatment options aim to alleviate pain and improve function without surgery. These methods focus on reducing inflammation, strengthening the spine, and promoting healing.
Physical Therapy
Physical therapy involves exercises and manual techniques to:
- Reduce pain and inflammation
- Improve range of motion and flexibility
- Strengthen the muscles supporting the spine
- Correct posture and movement patterns
Chiropractic Care
Chiropractors use spinal adjustments and other techniques to:
- Realign the spine and reduce pressure on the nerves
- Improve nerve function and blood flow
- Reduce pain and inflammation
Pain Medication
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce pain and inflammation. In some cases, prescription pain medication may be necessary.
Lifestyle Modifications
Lifestyle changes can also help manage symptoms:
- Maintaining a healthy weight:Excess weight puts strain on the spine.
- Regular exercise:Strengthening core and back muscles supports the spine.
- Proper posture:Avoid slouching or sitting in awkward positions for extended periods.
- Ergonomic workplace:Ensure your desk, chair, and other equipment are adjusted for optimal posture.
Surgical Treatment Options for Disc Herniation
Surgical intervention may be necessary for disc herniations that do not respond to conservative treatment or cause severe neurological deficits. The type of surgical procedure chosen depends on the location and severity of the herniation, as well as the patient’s overall health.
Surgical Techniques
- Microdiscectomy:This is the most common surgical procedure for disc herniations. It involves removing the herniated portion of the disc through a small incision in the back.
- Laminectomy:This procedure involves removing a portion of the lamina, the bony roof of the spinal canal, to create more space for the spinal cord and nerves.
- Fusion:In some cases, fusion surgery may be necessary to stabilize the spine and prevent further herniations. This involves fusing two or more vertebrae together using bone grafts or other materials.
Indications and Contraindications
Indications for surgery include:
If you’re struggling with a herniated disc, it’s essential to seek professional medical advice. While you’re at it, why not take a break and learn about business strategies with this insightful Swot Analysis For Toms Shoes ? When you return to your herniated disc recovery journey, you’ll have a fresh perspective and a deeper understanding of how to manage your condition effectively.
- Severe pain that does not respond to conservative treatment
- Progressive neurological deficits, such as weakness, numbness, or difficulty walking
- Cauda equina syndrome, a rare but serious condition that can cause paralysis of the legs and loss of bowel and bladder function
Contraindications to surgery include:
- Active infection
- Severe medical conditions that make surgery risky
- Patient refusal
The decision of whether or not to undergo surgery for a disc herniation is a complex one that should be made in consultation with a qualified neurosurgeon or orthopedic surgeon.
Recovery and Rehabilitation after Disc Herniation Treatment
Recovery after disc herniation treatment varies depending on the severity of the herniation and the type of treatment received. Conservative treatment typically involves a period of rest, followed by physical therapy and exercises to strengthen the muscles around the spine and improve flexibility.
Surgical treatment may require a longer recovery period, with restrictions on activity for several weeks or months.
Physical Therapy and Exercises
Physical therapy plays a crucial role in the rehabilitation process after disc herniation treatment. A physical therapist will design a personalized exercise program to help improve range of motion, strengthen the muscles around the spine, and reduce pain. Exercises may include:
– Stretching to improve flexibility – Core strengthening exercises to stabilize the spine – Aerobic exercises to improve cardiovascular health – Proprioceptive exercises to improve balance and coordination
Prevention and Management of Disc Herniations
Disc herniations are a common cause of back pain and other symptoms. While some risk factors for disc herniations are not modifiable, such as age and genetics, there are several things you can do to reduce your risk of developing a herniated disc and to manage an existing herniation to prevent recurrence.
Modifiable Risk Factors for Disc Herniations
- Smoking: Smoking damages the discs in your spine, making them more likely to herniate.
- Obesity: Excess weight puts extra stress on your spine, increasing your risk of a disc herniation.
- Poor posture: Sitting or standing with poor posture can put strain on your spine, leading to a disc herniation.
- Repetitive heavy lifting: Lifting heavy objects repeatedly can put strain on your spine and increase your risk of a disc herniation.
- Lack of exercise: Weak back muscles can make your spine more vulnerable to injury, including disc herniations.
Recommendations for Preventing Disc Herniations
There are several things you can do to reduce your risk of developing a disc herniation, including:
- Quit smoking: If you smoke, quitting is one of the best things you can do for your overall health, including your spine.
- Maintain a healthy weight: If you are overweight or obese, losing weight can help reduce the stress on your spine and lower your risk of a disc herniation.
- Practice good posture: When sitting or standing, make sure to keep your back straight and your shoulders relaxed. Avoid slouching or hunching over.
- Lift heavy objects properly: When lifting heavy objects, bend your knees and lift with your legs, not your back. Avoid twisting your back while lifting.
- Strengthen your back muscles: Regular exercise can help strengthen your back muscles and make your spine more resistant to injury.
Strategies for Managing Existing Disc Herniations
If you have an existing disc herniation, there are several things you can do to manage your symptoms and prevent recurrence, including:
- Rest: Resting your back can help reduce inflammation and pain.
- Apply ice or heat: Applying ice or heat to your back can help reduce pain and inflammation.
- Take over-the-counter pain relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce pain and inflammation.
- See a physical therapist: A physical therapist can teach you exercises to strengthen your back muscles and improve your posture.
- Consider surgery: Surgery may be an option if your symptoms are severe and do not respond to conservative treatment.
Common Queries
Thoát vị đĩa đệm có nguy hiểm không?
Thoát vị đĩa đệm có thể gây đau và khó chịu đáng kể, nhưng thường không nguy hiểm đến tính mạng. Tuy nhiên, trong một số trường hợp, thoát vị đĩa đệm có thể chèn ép tủy sống hoặc các dây thần kinh, dẫn đến các vấn đề nghiêm trọng hơn như tê liệt hoặc mất kiểm soát ruột.
Thoát vị đĩa đệm có thể tự khỏi không?
Trong một số trường hợp, thoát vị đĩa đệm có thể tự khỏi theo thời gian. Tuy nhiên, điều này không phải lúc nào cũng xảy ra và các triệu chứng có thể kéo dài trong nhiều tuần hoặc thậm chí nhiều tháng.
Điều trị sớm là rất quan trọng để giảm đau và ngăn ngừa các biến chứng.
Phẫu thuật thoát vị đĩa đệm có hiệu quả không?
Phẫu thuật thoát vị đĩa đệm có thể là một lựa chọn hiệu quả để giảm đau và cải thiện chức năng ở những người bị thoát vị đĩa đệm nghiêm trọng. Tuy nhiên, phẫu thuật không phải luôn cần thiết và các phương pháp điều trị bảo tồn, chẳng hạn như vật lý trị liệu và tiêm thuốc, có thể hiệu quả trong nhiều trường hợp.